Health
The Orchestrated Healing: How Cutting-Edge Care Coordination Approaches Are Streamlining Pathways for Superior Patient Outcomes
Introduction
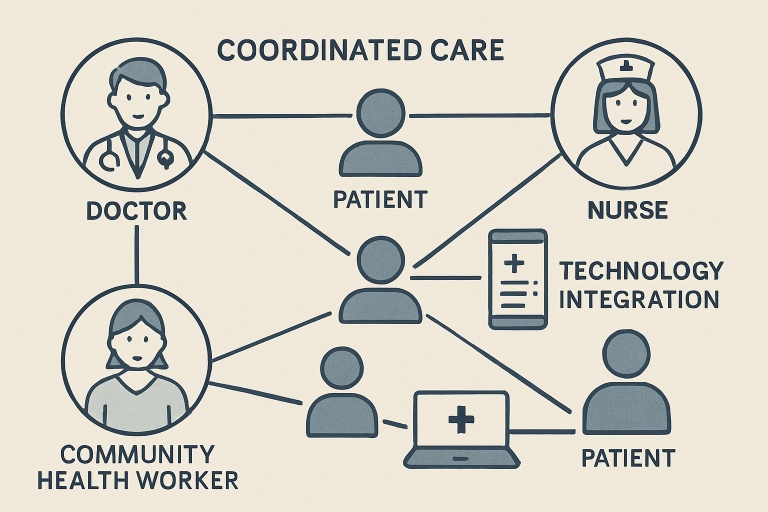
Effective care coordination is the foundation for delivering patient-centered healthcare across today’s diverse landscape. As patients and their families often navigate a maze of providers, specialists, and services, seamless coordination ensures that all aspects of a patient’s care are thoughtfully managed. This harmonization minimizes fragmentation and closes gaps that can lead to missed diagnoses, unnecessary duplication of services, and preventable adverse events. In recent years, the imperative for robust care coordination has intensified, driven by increasing patient needs, rising healthcare costs, and growing recognition of the social determinants of health. By embracing modern care coordination services and innovative approaches, health systems can create sustainable improvements in patient health, efficiency, and equity.
Integrating comprehensive care coordination strategies empowers healthcare teams to optimize the connections between patient needs, medical and community services, and long-term wellness goals. Beyond the technical aspects of record sharing and scheduling, true coordination incorporates people-centered outreach, personalized care planning, and ongoing assessments that adapt to changes in circumstances or treatment plans. These strategies foster proactive intervention, timely follow-up, and a holistic view of the patient, ultimately benefiting individuals, providers, payers, and entire communities.
Integrating Community Health Workers into Care Teams
Community health workers (CHWs) play an increasingly vital role as connectors, bridging the gap between medical systems and patients in need. By embedding CHWs into multidisciplinary care teams, health organizations can extend their reach into the communities they serve, particularly those with heightened social risks such as food insecurity, unstable housing, and limited access to transportation. CHWs serve as trusted liaisons who promote health literacy, navigate social services, and build lasting relationships that encourage patients to stay engaged with their care plans.
One real-world success story is Ohio’s Better Health Pathways HUB. This initiative has demonstrated measurable gains in patient well-being, provider satisfaction, and financial sustainability. By leveraging CHWs to coordinate comprehensive support, including linkage to food banks, housing assistance, and transportation, patients received more holistic care while care teams managed resources more effectively. The HUB not only improved care navigation but also generated significant Medicaid reimbursements, further validating the economic viability of this model. These outcomes showcase how integrating CHWs leads to better engagement, reduced disparities, and improved health outcomes on both the individual and system levels.
Leveraging Technology for Enhanced Care Coordination
Technological innovation is transforming care coordination by enabling the exchange of real-time information and facilitating seamless transitions across various care environments. Digital health platforms and AI-driven tools facilitate secure information exchange, allowing for proactive monitoring and personalized outreach. AI-based digital assistants help patients feel supported and empowered. At the same time, automated alerts, telehealth check-ins, and mobile health apps enable care teams to respond quickly to evolving needs and enhance care delivery.
Collaborative Models Between Primary Care and Specialists
Seamless collaboration between primary care providers (PCPs) and specialists is a linchpin of successful care coordination, especially for patients with chronic or complex illnesses. Coordinated models ensure that each provider, regardless of specialty, operates from a shared care plan with clear communication protocols, thereby reducing the likelihood of missed information, duplicative testing, or misaligned medication regimens. This unified approach streamlines patient care, eliminates confusion, and supports more accurate and timely interventions.
The oncology arena offers a compelling example, as illustrated by the National Comprehensive Cancer Network (NCCN). Here, close partnerships between PCPs and oncology specialists foster tailored patient journeys, from early detection through survivorship. Collaborative pathways ensure prompt escalation of care, unified medication management, and seamless transitions between outpatient and inpatient sites. By focusing all team members on clear, patient-centered goals, collaborative models elevate care quality, minimize risks, and enhance patient satisfaction. These structures also empower patients to better understand their care plans, which in turn improves outcomes and fosters trust in the healthcare system.
Implementing Care Coordination Models in Practice
Translating best practices in care coordination from theory into everyday operations requires structured models, commitment to training, and ongoing measurement of results. The Camden Coalition’s care management initiative exemplifies these principles by focusing on individuals with high medical and social needs who frequently use emergency or inpatient care. Through a patient-centered approach, organizing services around each individual’s goals and priorities, the coalition facilitates everything from primary care appointments and prescription refills to housing support and vocational programs.
The results have been striking: the program increased primary care follow-up utilization and contributed to fewer avoidable hospitalizations and complications, particularly among vulnerable populations. This model demonstrates that applying intentional, data-driven coordination not only improves patient satisfaction and health outcomes but also helps health systems use resources more efficiently. Proving both feasible and impactful, such approaches can be adapted across diverse communities and patient populations. Discover more about the Camden Coalition’s care coordination model.
Addressing Health Inequities Through Care Coordination
As the healthcare industry advances, care coordination is emerging as a crucial lever for addressing long-standing health inequities. By tailoring care approaches to reflect the unique needs, cultures, and contexts of local populations, health systems can break down barriers to access and improve outcomes where needs are greatest. Maryland’s Health Enterprise Zone project highlights the success of equitable care coordination, training local CHWs, opening patient-centered medical homes, and strengthening collaboration between public health and clinical care. These efforts produced measurable reductions in hospital utilization and improved patient satisfaction among underserved communities. By focusing on cultural competence, outreach, and integration of community-based supports, these forward-thinking care coordination models propel health equity and advance population health. The key insight is that closing social gaps and reducing disparities is possible when innovation and commitment are matched by tailored, community-driven strategies that address each patient’s full range of needs.
























